Why Measuring Cardiometabolic Risk is Important to You
We all know that diseases like type 2 diabetes, cardiovascular disease and metabolic syndrome are bad and that catastrophic health events like a heart attack or stroke are really bad. Many of the personal risk factors that drive these diseases and events are largely driven by dietary and lifestyle choices we have made. As such, preventing and managing risk for them is also largely modifiable.
Modifying individual risk starts with early, precision identification.
First, 10 facts about cardiometabolic disease that you may not realize:
Cardiovascular disease is the #1 leading cause of death for men and women in the U.S.
Every year, about 805,000 Americans have a heart attack.
About 2 in 10 deaths from coronary artery disease happen in adults less than 65 years old.
Someone in the United States has a stroke every 40 seconds. Every 4 minutes, someone dies of stroke.
Cardiovascular disease (including strokes) is the #1 leading cause of death for men and women in the U.S.
1 in 3 adults have at least 1 high risk factor for suffering a stroke: blood pressure, high cholesterol, smoking, obesity, and diabetes.
People with established cardiovascular disease spend an average of +$19,000 more annually on medical care.
Diabetes is the 7th leading cause of death in the U.S.
More than 88 million US adults—over a third—have prediabetes, and more than 84% of them don’t know they have it.
Medical costs for people with diabetes are 2x as high as for people who don’t have diabetes.
In today’s healthcare system, most clinical professionals just do not have the time or all of the tools to adequately assess each person’s risk for these costly and deadly diseases. They want to have the time and resources, they really do! But, because the data may be compartmentalized in electronic medical record (EMR) systems, the labs available may be estimates instead of the most accurate biomarkers, and because the guidelines that drive clinical decision-making to assess risk are ever-changing it’s often not possible in a typical 15-30 minute clinical encounter.
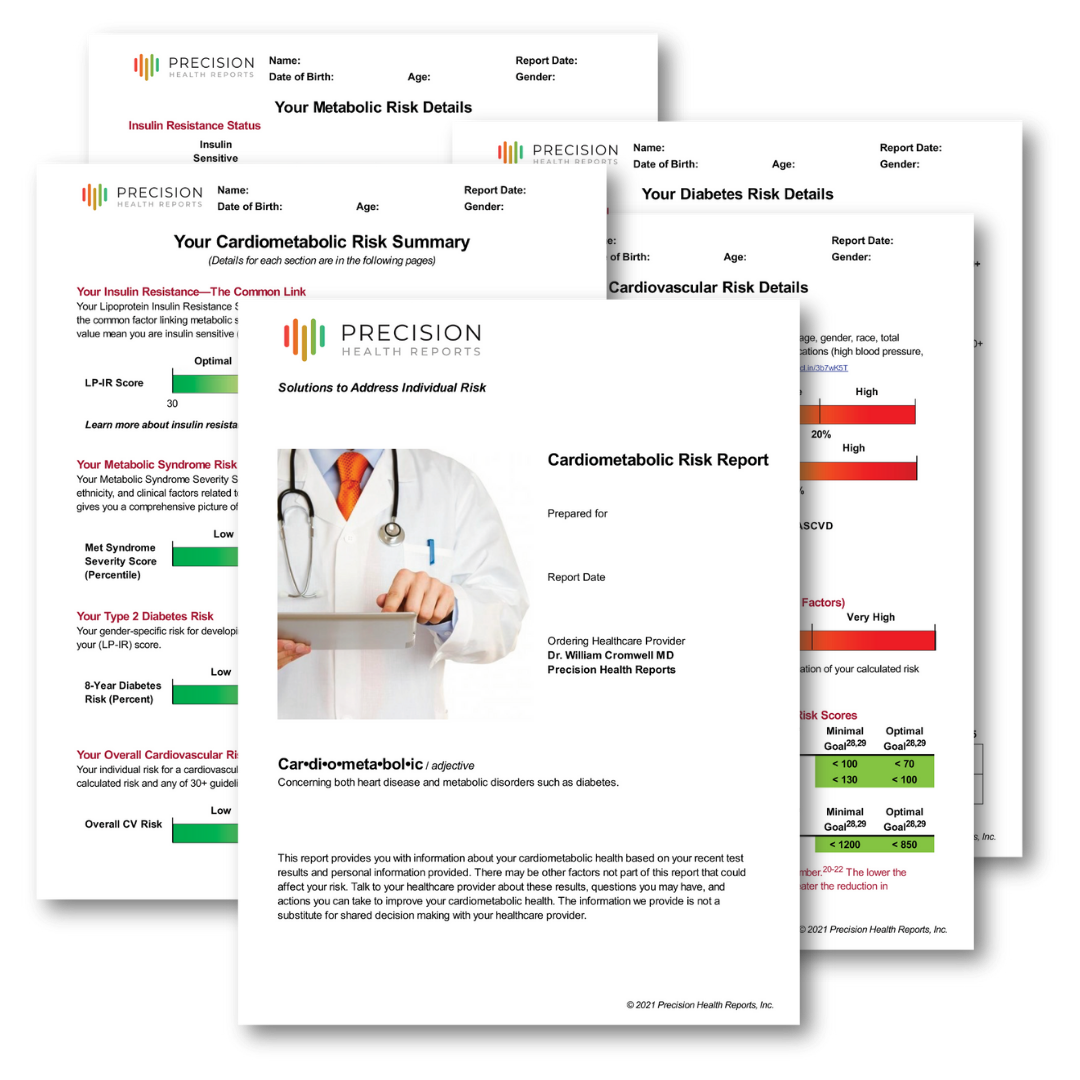
Our risk assessment reports fill a critical need for a personalized, understandable, actionable report for your risk of heart attack, stroke, and diabetes. We are built to enable individuals, doctors, allied health professionals, and health coaches to exercise proper shared decision-making with regard to these costly and deadly conditions with the necessary, best tools available for the job.
The Backstory of Assessing and Managing Risk
Now like a lot of areas of medicine, the strategies for assessing and managing risk have evolved over time in response to decades of research. In the 1980s, our initial approach to identifying risk for cardiovascular events such as heart attack and stroke was based on studying large groups of people over many decades to find factors that seem to be common to individuals who had heart attacks or strokes. The common risk factors identified included age, gender, cholesterol levels, smoking, and hypertension. Now in separate studies, researchers looked for factors that would identify people at increased risk for developing diabetes over time. Diabetic risk factors included things like fasting glucose, body mass index, HDL cholesterol, family history of diabetes, triglycerides, and blood pressure. Based on this information, risk equations were developed to classify people as having low, moderate, or high risk of developing cardiovascular disease or diabetes. While this was a good start, a person's actual risk of diabetes, heart attack, or stroke was often very different from their assigned group. For example, many people identified as low risk were actually at much higher risk than at first expected. And, likewise, people who were classified a high risk frequently had much less risk than expected. These limitations of a risk factor based approach showed us that we were missing critical details such as how these conditions develop (e.g. what was the root cause), and what additional factors need to be included to identify individual risk.
Modern Risk Assessment
Over the past 3 decades, world wide research has improved our understanding of how these conditions develop, and what factors are missing. Now, multiple, national, and international guidelines exist that collectively use over 30 additional laboratory and clinical risk enhancing factors to improve our identification and management of individuals who are at risk for heart attack, and stroke. In terms of diabetic risk, we know now that type 2 diabetes develops over time in response to a condition known as insulin resistance, and insulin resistance combined with how well the pancreas produces insulin to overcome insulin resistance is really what's happening under the hood to put you at risk of diabetes. Knowing both of these central elements is critical to determining your risk of developing diabetes. We've also learned that cardiovascular disease and diabetes really aren't separate conditions, but they're connected by a common condition known as the insulin resistance syndrome. This new learning allows us to identify and manage one condition, the insulin resistance syndrome to improve simultaneously our prediction and management of your risk for heart attack, stroke, and diabetes. It's important to note that the insulin resistance syndrome can be really significantly improved with appropriate changes and diet and activity. So as insulin resistance improves, many of the factors that drive cardiovascular and diabetic risk also improve.
Now as you can imagine, trying to take all this complexity and distill it into a single, precise, understandable, actionable report one patient at a time is very challenging. Integrating national and international guidelines, laboratory data, clinical history, and more than two dozen risk enhancing factors to develop a single patient specific report is not only time consuming, but is a quite frankly is not doable for most clinicians in daily practice.
Why Precision Health Reports Does What We Do
That's why we developed Precision Health Reports: to provide personalized solutions to identify and manage risk for heart attack, stroke, and diabetes. We are built to take the complexity barriers, all too often present, and tear them down. We are built to simplify the process to make risk identification accessible. Our proprietary algorithm integrates all relevant clinical information, outcome proven clinical biomarker values, the relevant risk enhancing factors, as well as multiple national and international guidelines to produce your personalized, specific, actionable report. Not only does our Cardiometabolic Risk Assessment Report reveal an individual’s personalized risk and the critical values that amplify their risk, the report also identifies and tracks the laboratory values that are most predictive of risk reduction in response to diet, exercise, lifestyle, and medications.
How Often Should You Assess Risk
It depends (yes, no one actually likes that answer). Assessing your cardiometabolic disease risk is not a “one and done” event. You’ll want to assess periodically to measure progress and identify new risk factors before they become urgent. If the disease risk is low and well-managed then likely 8-12 months between assessments is a correct interval. If identified risk is high, very high or extremely high, and/or you are looking for more granular indications of biomarker and risk scores changing based on changes in lifestyle, diet, and medications, then perhaps as little as 3-6 month intervals are enough time to see the changes you are looking for. Assessments intervals less than three months are unlikely to show significant change.
Conclusion
Whether you are looking to take control of your own cardiometabolic risk or a healthcare practitioner that assesses risk for your patients, we are here to support you in finding risk early. Most Americans, sadly, have at least one risk factor for metabolic syndrome and are at risk for diabetes, heart attack, or stroke. Finding that risk early and doing something about it is the #1 way to stop disease progression.