Metabolic Syndrome Severity Score
One in three adults in the United States meets criteria for metabolic syndrome. Most don’t know it.
But risk doesn’t stop at a yes/no diagnosis. The Metabolic Syndrome Severity Score (MSSS) shows just how far along the disease pathway someone really is.
Metabolic syndrome is a cluster of risk factors—abdominal obesity, elevated blood pressure, high triglycerides, low HDL cholesterol, and impaired fasting glucose—that greatly increase the likelihood of type 2 diabetes, heart attack, and stroke (AHA overview). Traditionally, clinicians diagnose metabolic syndrome if three or more of these risk factors are present. But this “yes/no” approach misses the reality that risk exists on a continuum.
What is Metabolic Syndrome?
What Causes Metabolic Syndrome?
Metabolic syndrome occurs in response to a process known as insulin resistance. To understand insulin resistance, let’s start by looking at how things are designed to work. Normally, insulin from your pancreas works in liver cells, muscle cells and fat cells to regulate glucose and energy metabolism. When your insulin gets overwhelmed, it can cause added stress on your pancreas which leads to increased risk for developing type 2 diabetes.
Approximately 34% of the U.S. population has metabolic syndrome, and about 85% of individuals with type 2 diabetes have metabolic syndrome.
Metabolic syndrome is present in approximately 9% of people with normal body weight, 22% of those who are overweight and 60% of those considered obese. Adults who continue to gain five or more pounds per year raise their risk of developing metabolic syndrome by up to 45%.
The prevalence of metabolic syndrome increases with age, and about 50% of people over 60 are affected.
In the U.S., Hispanic Americans have the highest prevalence of metabolic syndrome.
How Common is Metabolic Syndrome?
How insulin works in liver cells, muscle cells, and fat cells
Why a Continuous Score Matters
Traditional definitions treat someone with three risk factors the same as someone with five, even though their true risk is very different. MSSS fills this gap by integrating all five components into a single, standardized score.
Stronger prediction of future disease: Higher MSSS values are linked with increased risk for type 2 diabetes and atherosclerotic cardiovascular disease.
Tracks improvement over time: Changes in MSSS reflect whether interventions like lifestyle, nutrition, or medication are lowering overall metabolic risk.
Validated across ethnicities: Studies show MSSS accurately predicts disease risk in diverse racial and ethnic groups, making it more reliable than specific cutoff values that may be non-specific and unweighted to the individual.
Similar to someone with three factors being treated the same as somone with five factors, the same holds true for individuals with only one or two factors. These pople would often fly under the radar as not having metabolic syndrome. Both if their triglycerides were very high and waist circumference were high, they would have a much higher risk than someone with one or two metabolic syndrome features that were lower.
Who should care about metabolic syndrome?
Adults who are overweight or have obesity (especially abdominal)
Anyone with prediabetes or insulin resistance
People with family history of type 2 diabetes, heart attack, or stroke
High-risk groups such as first responders and shift workers
The Metabolic Syndrome Severity Score (MSSS) is a validated tool that overcomes the limitations of the common categories approach. Instead of a binary diagnosis, it provides a continuous measure of metabolic health that reflects the severity of underlying risk. MSSS has been shown to predict the future development of type 2 diabetes and cardiovascular disease in multiple populations better than starndard yes/no criteria (PubMed abstract).
See Your True Risk
Basic lab panels can’t show your trajectory. Our Assessments use MSSS plus advanced biomarkers to reveal where you stand and how to change your future risk.
Calculate Your Own Metabolic Syndrome Severity score with the MSSS Calculator.
Metabolic Syndrome Severity Score Calculator
Enter your values below. Units: inches / pounds. Results are informational only.
Gurka, M. J., Lilly, C. L., Oliver, M. N., & DeBoer, M. D. (2014). An examination of sex and racial/ethnic differences in the metabolic syndrome among adults: a confirmatory factor analysis and a resulting continuous severity score. Metabolism, 63(2), 218-225.
Gurka, M. J., DeBoer, M., Filipp, S., Khan, J., Rapczak, T. J., Braun, N. D., Hanson, K. S., & Barnes, C. P. (2019). MetS Calc: Metabolic Syndrome Severity Calculator. doi: 10.5281/zenodo.2542213
Beyond MSSS: A More Complete Picture
While MSSS is powerful, it is only one part of understanding metabolic and cardiovascular health. Important risk factors like ApoB, LDL-P, Lipoprotein(a), and LP-IR also provide outcome-proven insights into cardiometabolic risk.
That’s why at Precision Health Reports, we integrate MSSS with advanced biomarkers, ethnicity-specific thresholds, and harmonized clinical guidelines. This allows us to go beyond a single score and deliver a comprehensive, personalized risk profile. Establishing a precise metabolic syndrome baseline ensures that we can provide you with an accurate picture of health upstream progression to pre-diabetes or type 2 diabetes.
Metabolic syndrome risk for heart attack, stroke, and type 2 diabetes
Heart attack and stroke risk increases with the number of metabolic syndrome factors present. Compared to those with no metabolic syndrome factors, heart attack and stroke are increased 4-fold for men and 6-fold for women who have 3 or more factors.
Likewise, diabetes risk increases with the number of metabolic syndrome factors present. Compared to those with no metabolic syndrome factors, risk of developing diabetes is 24-fold higher for men and 30-fold higher for women who have 3 or more factors.
📚Data from multiple landmark studies, including the Atherosclerosis Risk in Communities Study, Jackson Heart Study, and the National Diabetes Prevention Program (DPP), show a significant relationship between higher Metabolic Syndrome Severity Scores and risk for heart attack, stroke, and diabetes.
Do individuals with the same number of metabolic syndrome factors have the same risk?
Actually, NO. Counting the number of factors is not the same as knowing the actual measured value for a factor. For example, let’s compare a person with fasting blood sugar of 100 mg/dL and someone with a fasting blood sugar of 200 mg/dL. Both people meet criteria for having a metabolic syndrome factor (fasting blood sugar > 100 mg/dL). But, the higher the measured value, the greater the individual risk. The Metabolic Syndrome Severity Score overcomes this problem by giving a precise scale from 0-100 to get the clearest picture of metabolic syndrome risk.
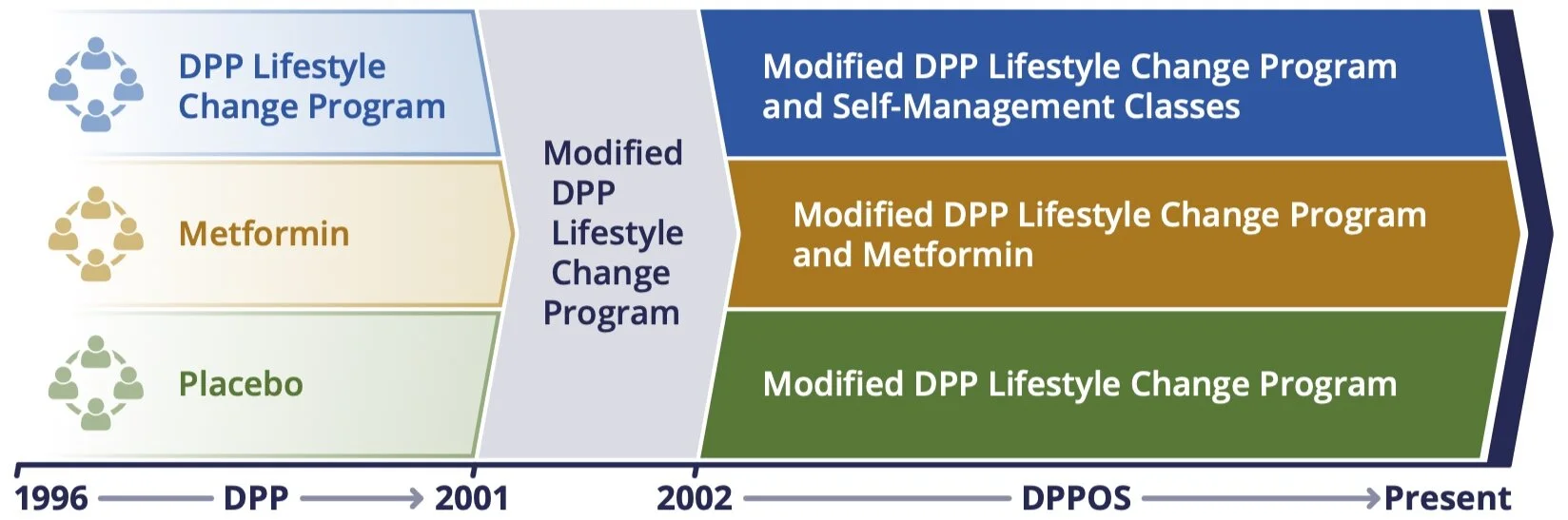
Diabetes Prevention Program (DPP) and ongoing DPP Outcomes Study (DPPOS)
What to Remember about Metabolic Syndrome (and the MSSS)
Metabolic Syndrome is a precursor to risk for developing type 2 diabetes and cardiovascular disease.
Metabolic syndrome is typically measured with 5 categorical factors, but those are insensitive to magnitude.
The Metabolic Syndrome Severity Score is a significantly more granular representation of individual risk for metabolic syndrome.
Take the Next Step
The Metabolic Syndrome Severity Score is an important foundation, but don’t stop there. Our Advanced Metabolic Health Assessment and Cardiometabolic Risk Assessment combine MSSS with deeper biomarkers and guideline-driven recommendations to give you a clear path forward.
FAQs for the Metabolic Syndrome Severity Score
-
The Metabolic Syndrome Severity Score is a validated tool that measures the severity of metabolic syndrome on a continuous scale rather than a simple yes/no diagnosis. Higher scores indicate greater risk for developing type 2 diabetes, heart attack, or stroke.
-
A traditional diagnosis only confirms whether someone meets three or more criteria for metabolic syndrome. MSSS integrates all five risk factors into a single score, providing a more precise way to track risk and progress over time.
-
MSSS is useful for adults with overweight or obesity, prediabetes, insulin resistance, or family history of type 2 diabetes and cardiovascular disease. It’s also valuable for high-risk groups such as first responders, shift workers, and people with multiple lifestyle risk factors.
-
Yes. Studies show that improvements in weight, blood pressure, blood sugar, and lipids can lower MSSS over time. This makes MSSS a valuable way to measure the impact of lifestyle changes and treatment.
-
MSSS is an excellent marker but it should be combined with other outcome-proven biomarkers like ApoB, LDL-P, Lipoprotein(a), and LP-IR. Precision Health Reports integrates MSSS with these advanced measures to give a more complete view of risk.
-
We include MSSS as part of our Advanced Metabolic Health Assessment and Cardiometabolic Risk Assessment. This ensures your results are interpreted in context, with guideline-driven recommendations tailored to your personal risk.
References
Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med 2011;9:48-.
Moore JX, Chaudhary N, Akinyemiju T. Metabolic Syndrome Prevalence by Race/Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis 2017;14:E24-E.
Lau DCW, Yan H, Dhillon B. Metabolic syndrome: a marker of patients at high cardiovascular risk. Can J Cardiol 2006;22 Suppl B:85B-90B.
Marc J. Genetic Susceptibility to Metabolic Syndrome. EJIFCC 2007;18:7-14.
Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the Metabolic Syndrome in the United States, 2003-2012. JAMA 2015;313:1973-4.
Wilson PWF, D’Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic Syndrome as a Precursor of Cardiovascular Disease and Type 2 Diabetes Mellitus. Circulation 2005;112:3066-72.
Gurka MJ, Golden SH, Musani SK, et al. Independent associations between a metabolic syndrome severity score and future diabetes by sex and race: the Atherosclerosis Risk In Communities Study and Jackson Heart Study. Diabetologia 2017;60:1261-70.
Gurka MJ, Guo Y, Filipp SL, DeBoer MD. Metabolic syndrome severity is significantly associated with future coronary heart disease in Type 2 diabetes. Cardiovasc Diabetol 2018;17:17.
DeBoer MD, Filipp SL, Gurka MJ. Use of a Metabolic Syndrome Severity Z Score to Track Risk During Treatment of Prediabetes: An Analysis of the Diabetes Prevention Program. Diabetes Care 2018;41:2421-30.
Lanier JB, Bury DC, Richardson SW. Diet and Physical Activity for Cardiovascular Disease Prevention. Am Fam Physician 2016;93:919-24.
Kitabchi AE, Temprosa M, Knowler WC, et al. Role of insulin secretion and sensitivity in the evolution of type 2 diabetes in the diabetes prevention program: effects of lifestyle intervention and metformin. Diabetes 2005;54:2404-14.
learn more about the Metabolic Syndrome calculator for juveniles at https://www.ncbi.nlm.nih.gov/pubmed/23062212 or adults at https://www.ncbi.nlm.nih.gov/pubmed/24290837