ApoB vs. LDL-C: Why the Numbers Don’t Always Match
ApoB vs. LDL Cholesterol: Which Tells the Real Story?
For decades, LDL cholesterol (LDL-C) has been the standard lab marker used to assess cardiovascular risk. But research has made it clear that apolipoprotein B (ApoB) is a more accurate measure of risk because it directly reflects the number of particles driving plaque formation.
The mismatch between ApoB and LDL-C, called discordance, can leave patients at risk even when their LDL-C looks “normal.” Let’s break down why these numbers don’t always match, how each is measured, and why ApoB should be front and center in modern risk assessment. The similiar terminology of “LDL” and “LDL-C” also contributes to the confusion. Let’s dive in!
What ApoB Actually Measures
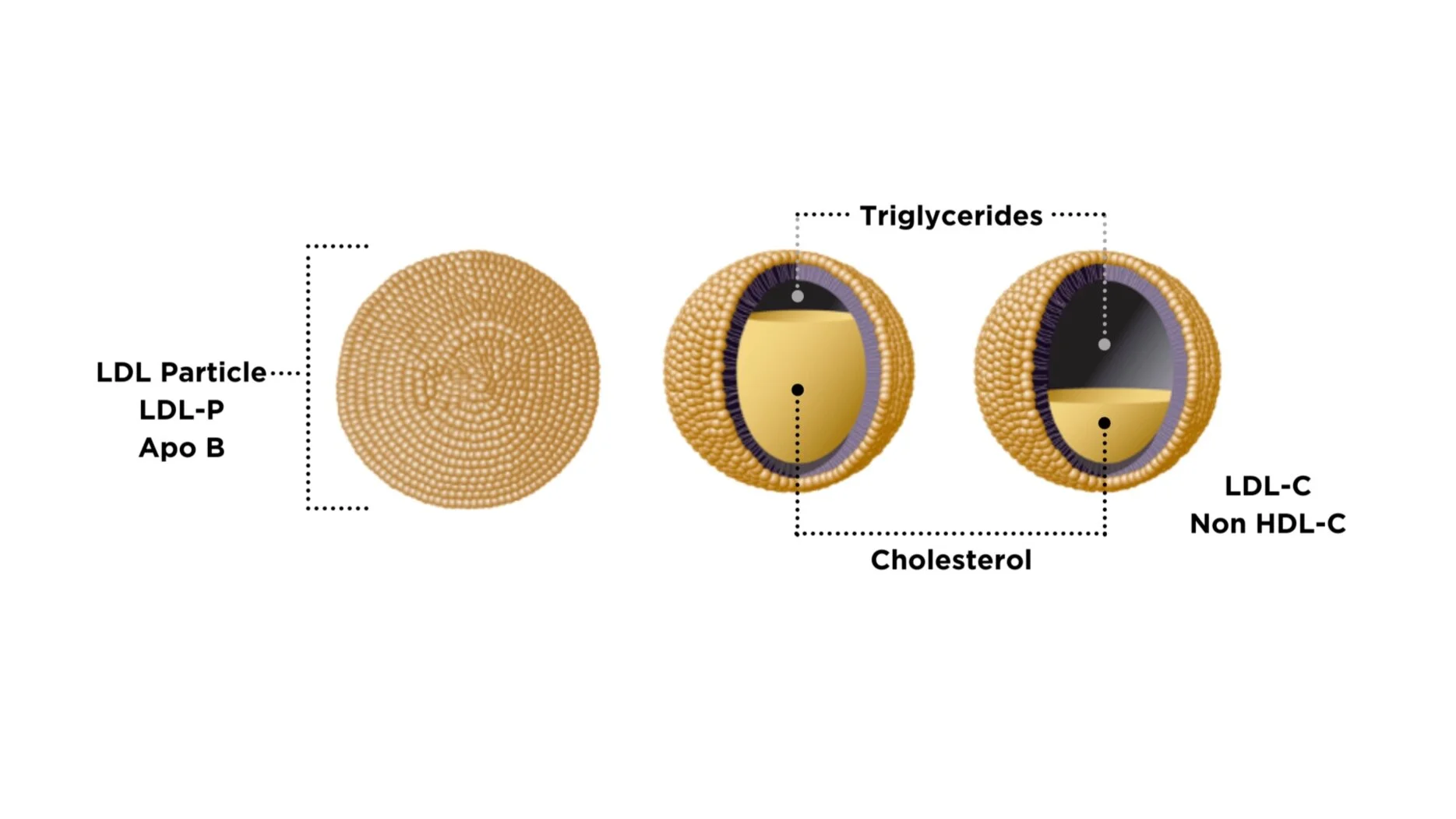
Every atherogenic lipoprotein particle (LDL, VLDL, IDL, and Lp(a)) carries a single ApoB molecule. That means ApoB is essentially a particle count. The higher your ApoB, the more cholesterol-carrying particles are circulating in your bloodstream, and the higher your risk of atherosclerosis.
Unlike LDL-C, measuring ApoB is not about how much cholesterol is inside the particles. Instead, it’s about how many particles there are. Since plaque risk is driven by the number of artery-penetrating particles, ApoB provides a truer signal of risk.
➡ Related reading: What You Need to Know About Your Atherogenic Particle Number (LDL-P or ApoB)
Figure 1: Think of your arteries like a road. When you want to identify traffic, do you count the number of people or the number of vehicles? Vehicles, of course! The number of people in the vehicles is variable and reducing the number of vehicles reduces your traffic. With this analogy, ApoB is the number of vehicles while LDL-C is the variable number of people in the vehicle. Reduce the number of vehicles!
How ApoB Is Accurately Measured Using NMR Technology
Modern labs (including LabCorp used by Precision Health Reports for all of our Assessments) use nuclear magnetic resonance (NMR) spectroscopy to directly measure lipoprotein particle numbers. This method detects signals from the lipoproteins in blood and quantifies particle concentrations, including ApoB-containing LDL, VLDL, and IDL particles.
Other methods, such as immunoassays, also exist and provide strong accuracy. But NMR profiling gives unmatched precision in most accurately distinguishing particle sizes and numbers. Particle size differences can indicate risk for insulin resistance that gets measured in the Lipoprotein Insulin Resistance Score (LP-IR). portion of the Risk Assessment reports.
How LDL-C Gets Measured (and Its Limitations)
LDL-C is not usually measured directly—it’s often calculated:
Friedewald Equation: LDL-C = Total Cholesterol – HDL-C – (Triglycerides ÷ 5).
Cheap and widely used.
Inaccurate when triglycerides are high (>400 mg/dL).
Martin/Hopkins Method: A more recent formula that adjusts for triglyceride levels.
Direct LDL-C assays: Available but more expensive and still measure cholesterol content, not particle count.
The problem? LDL-C is an estimate of cholesterol mass, not the actual number of LDL particles. People with the same LDL-C can have very different ApoB levels depending on particle size and distribution.
When ApoB and LDL-C Don’t Match: The Problem of Discordance
Here’s where patients get into trouble:
Normal LDL-C but high ApoB: Cholesterol content looks fine, but there are too many particles. This is especially common in insulin resistance, metabolic syndrome, and type 2 diabetes.
High LDL-C but normal ApoB: Cholesterol content looks high, but the number of particles is not as concerning.
Multiple large studies show that ApoB predicts cardiovascular events more accurately than LDL-C when they disagree.
LDL vs. LDL-C: Clearing Up the Confusion
The terms “LDL” and “LDL-C” are often used interchangeably, but they are not the same:
LDL = the particle itself (a carrier of cholesterol, triglycerides, and ApoB).
LDL-C = the cholesterol mass inside those particles.
This subtle distinction confuses patients and sometimes is exploited by those claiming “LDL doesn’t matter.” The truth is that LDL particle number (ApoB) is what drives risk definitely matters. LDL-C can sometimes under- or overestimate risk so that leads to much of the confusion.
Why Social Media Influencers Often Mislead on LDL
If you scroll through health social media, you’ve likely seen claims like “LDL is harmless” or “high cholesterol is not dangerous.”
The problem is that many of these arguments cherry-pick LDL-C data, ignoring particle science. Some even conflate total cholesterol, LDL, and LDL-C to downplay risk. While it makes for catchy content, it’s misleading and potentially dangerous.
The scientific consensus is clear: atherogenic particle number (ApoB) is the causal driver of plaque.
Why This Matters for Your Heart Health
If your risk assessment relies only on LDL-C, you could be given false reassurance. Patients with diabetes, obesity, or metabolic syndrome are especially prone to LDL-C/ApoB discordance.
That’s why Precision Health Reports includes ApoB in every Cardiometabolic Risk Assessment: to ensure no hidden risk is overlooked.
➡ See how the Cardiometabolic Risk Assessment gives you a complete picture.
The Bottom Line: ApoB vs. LDL-C
ApoB = particle count (direct, accurate, predictive).
LDL-C = cholesterol mass estimate (indirect, sometimes misleading).
When they disagree, trust ApoB because it better reflects true risk.
FAQs about ApoB and LDL-C
1. What is the difference between ApoB and LDL-C? ApoB measures the number of atherogenic particles in your blood, while LDL-C measures the amount of cholesterol inside those particles. ApoB is a more accurate predictor of heart disease risk.
2. Why is ApoB more accurate than LDL-C? Because each atherogenic particle (LDL, VLDL, IDL, Lp(a)) carries one ApoB protein, measuring ApoB directly reflects how many cholesterol-carrying particles are circulating. LDL-C can underestimate risk, especially in people with insulin resistance or diabetes.
3. Can I have normal LDL-C but high ApoB? Yes. This is called discordance, and it happens when the number of LDL particles is high but each carries a variable amount of cholesterol. Patients with discordance are at higher risk for heart disease even if their LDL-C looks “normal.”
4. How is ApoB measured? ApoB is measured with a blood test, often using immunoassay or advanced methods like nuclear magnetic resonance (NMR) profiling. These provide a direct and reliable measure of particle number.
5. Why do doctors still use LDL-C instead of ApoB? LDL-C has been used for decades and is inexpensive, so it remains common in standard labs. However, major medical societies (ACC, AHA, ESC, NLA) increasingly recognize ApoB as a superior marker and recommend it for patients at higher risk.
6. What should I do if my LDL-C is normal but my ApoB is high? Talk to your healthcare provider about your full cardiometabolic risk profile. Treatments such as lifestyle changes and lipid-lowering therapies can be guided more precisely when ApoB is measured.
📚 Further Reading on ApoB and LDL-C
2018 ACC/AHA Cholesterol Guidelines
The official U.S. cholesterol management guideline. Highlights the role of ApoB and non-HDL cholesterol as stronger risk predictors than LDL-C.
Sniderman AD, et al. – JAMA Cardiology Review (2019)
A concise review explaining why ApoB is the most accurate marker of atherogenic particle number and should guide clinical decision-making.
Mora S, et al. – Circulation Study (2014)
Showed that when LDL-C and ApoB are discordant, ApoB is the better predictor of future coronary events.
Wilkins JT, et al. – JAMA Study (2016)
Young adults with normal LDL-C but high ApoB were more likely to develop coronary artery calcification, highlighting the hidden risks of relying on LDL-C alone.
Ference BA, et al. – European Heart Journal (2017)
Genetic and clinical evidence proving LDL particles cause atherosclerosis, with ApoB as the best reflection of particle number.


