GlycA: A Biomarker of Chronic Inflammation
A stable blood-based measure that captures systemic, low-grade inflammation linked to cardiometabolic disease, long-COVID, autoimmune activity, and all-cause mortality.
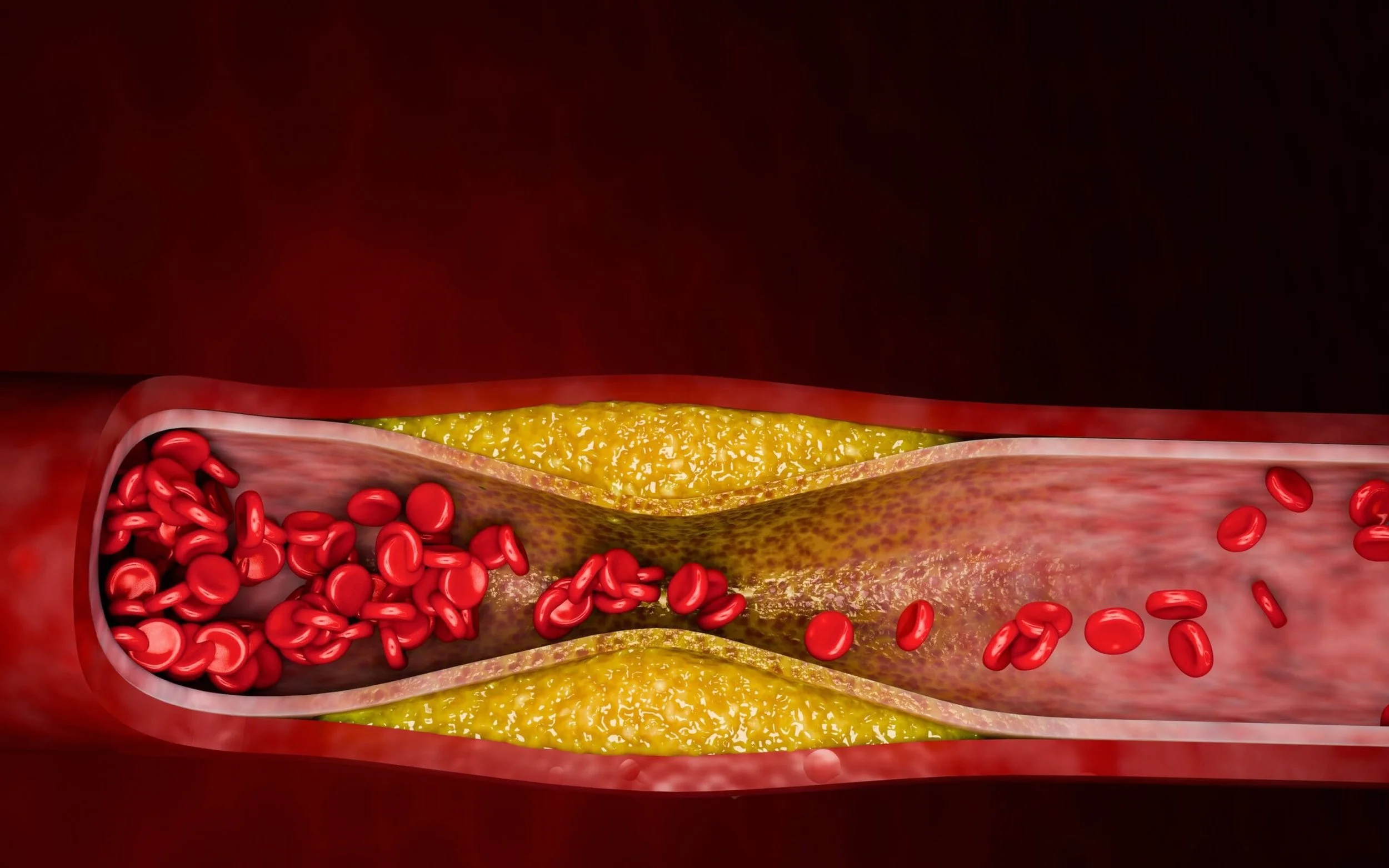
GlycA is an advanced inflammatory biomarker derived from NMR spectroscopy. Unlike hs-CRP—an acute-phase inflammation marker—GlycA reflects chronic, persistent inflammation originating from the glycosylated proteins of the innate immune system. Research shows GlycA strongly predicts cardiometabolic disease, type 2 diabetes, ASCVD events, hospitalization risk, and mortality, making it one of the most clinically useful long-term inflammation markers available today. Precision Health Reports incorporates GlycA into comprehensive risk assessment because it provides a more reliable view of metabolic and vascular inflammation, especially in patients with metabolic syndrome, obesity, insulin resistance, or chronic fatigue-like syndromes.
What is GlycA?
GlycA (Glycoprotein Acetylation) is a composite biomarker derived from the NMR signal of several acute-phase glycoproteins—primarily α1-acid glycoprotein, haptoglobin, α1-antitrypsin, transferrin, and α1-antichymotrypsin. These proteins circulate at stable baseline levels and rise with chronic inflammatory signaling.
Fast Facts
Reflects chronic, systemic inflammation
More stable day-to-day than hs-CRP (less biological variability)
Predicts cardiometabolic, autoimmune, and infectious disease risk
Not affected by short-term infections the way hs-CRP is
Why GlycA Matters
GlycA adds diagnostic clarity in situations where other inflammation markers may be incomplete or misleading. Elevated GlycA levels correlate with:
Increased ASCVD event risk
Higher likelihood of developing type 2 diabetes
Systemic metabolic dysfunction and insulin resistance
Chronic inflammatory conditions (long-COVID, ME/CFS, autoimmune activity)
Higher all-cause mortality in population studies
Because chronic inflammation is central to cardiometabolic disease, GlycA strengthens risk stratification and reveals inflammatory contribution even when traditional biomarkers appear normal.
What Guidelines Say
While no major U.S. guideline (ACC/AHA, ADA) has standardized GlycA as a routine inflammation measure, peer-reviewed evidence consistently supports its value in chronic inflammatory burden and long-term disease prediction. Several organizations, including Cleveland HeartLab and LabCorp, have incorporated GlycA into inflammation panels.
Clinicians increasingly use GlycA as:
A risk-enhancing factor for ASCVD risk discussion
A metabolic inflammation marker to identify cardiometabolic dysfunction
A monitoring tool during lifestyle or pharmacologic therapy (GLP-1s, anti-inflammatories, weight loss interventions)
As research grows, GlycA is becoming a go-to tool for understanding chronic inflammatory load.
How GlycA Is Measured
GlycA is measured using NMR spectroscopy, which quantifies the concentration and glycosylation patterns of circulating glycoproteins. Results are typically reported in µmol/L.
Interpretation is straightforward:
Low / Optimal: < 400 µmol/L
High: 400+ µmol/L
Severity correlates with long-term inflammatory burden and metabolic dysfunction.
What Causes Elevated GlycA?
Common underlying drivers include:
Insulin resistance and metabolic syndrome
Obesity and visceral adiposity
Chronic infections or post-viral conditions (including long-COVID)
Autoimmune or rheumatologic diseases
Chronic stress and poor sleep
Inflammatory dietary patterns
Smoking or chronic toxin exposure
Liver dysfunction
Poor cardiorespiratory fitness
GlycA is especially valuable because it identifies persistent inflammatory activity even when hs-CRP is normal or fluctuating.
GlycA vs hs-CRP
GlycA and hs-CRP are often compared, but they measure different physiological phenomena.
GlycA
Highly stable
Reflects chronic inflammation
Strong predictor of metabolic risk
Derived from glycoprotein acetylation signal
Useful in cardiometabolic, infectious, and fatigue-associated inflammation
hs-CRP
Fluctuates significantly
Reflects acute inflammation
Strong predictor of ASCVD risk
Influenced by recent illness, exercise, or injury
Some clinicians benefit from using both, but GlycA is more reliable for chronic inflammation profiling and is what is used exclusively in the Cardiometabolic Risk Assessment.
GlycA in Cardiometabolic Risk
For patients with:
Metabolic syndrome
Prediabetes
Obesity
Elevated ApoB or LDL-P
Elevated LP-IR
GlycA helps determine whether inflammation is contributing to their cardiometabolic trajectory.
Precision Health Reports uses GlycA as part of a comprehensive risk modeling system that incorporates:
ApoB
Lp(a)
LP-IR
GlycA
Fasting glucose
Advanced lipid testing
This allows clinicians to see both lipid-driven and inflammation-driven pathology.
FAQs about GlycA
-
They’re complementary. GlycA is more stable and reflects long-term inflammation. hs-CRP better captures acute spikes.
-
Typically >400 µmol/L is high risk for cardiometabolic disease and chronic inflammation.
-
Yes. It responds to weight loss, improved fitness, insulin sensitivity, and anti-inflammatory interventions.
-
esearch supports GlycA as a useful marker of persistent inflammatory load seen in post-viral syndromes, but nothing is definitive yet.
-
No. It is a specialty NMR test offered by limited labs (LabCorp, Cleveland HeartLab). It is included in the Precision Health Reports assessments.