Metabolic Syndrome: Beyond the Checklist with the Metabolic Syndrome Severity Score
Metabolic syndrome is one of the most important public health challenges of our time. Defined as a cluster of cardiometabolic risk factors, it dramatically increases the likelihood of developing type 2 diabetes, atherosclerotic cardiovascular disease (ASCVD), and stroke.
Traditionally, clinicians have used a binary checklist to diagnose metabolic syndrome: patients either have it (three or more risk factors) or they don’t. While useful, this approach is limited. It fails to capture the degree of severity and may underestimate future risk for many individuals.
That’s where the Metabolic Syndrome Severity Score (MSSS) comes in. The MSSS was developed through confirmatory factor analysis using comprehensive population data from NHANES (1999–2010), offering a robust and representative foundation for its continuous severity measurement. What it does in practice is that it provides a continuous, personalized measure of metabolic syndrome severity, adjusted for sex and race/ethnicity.
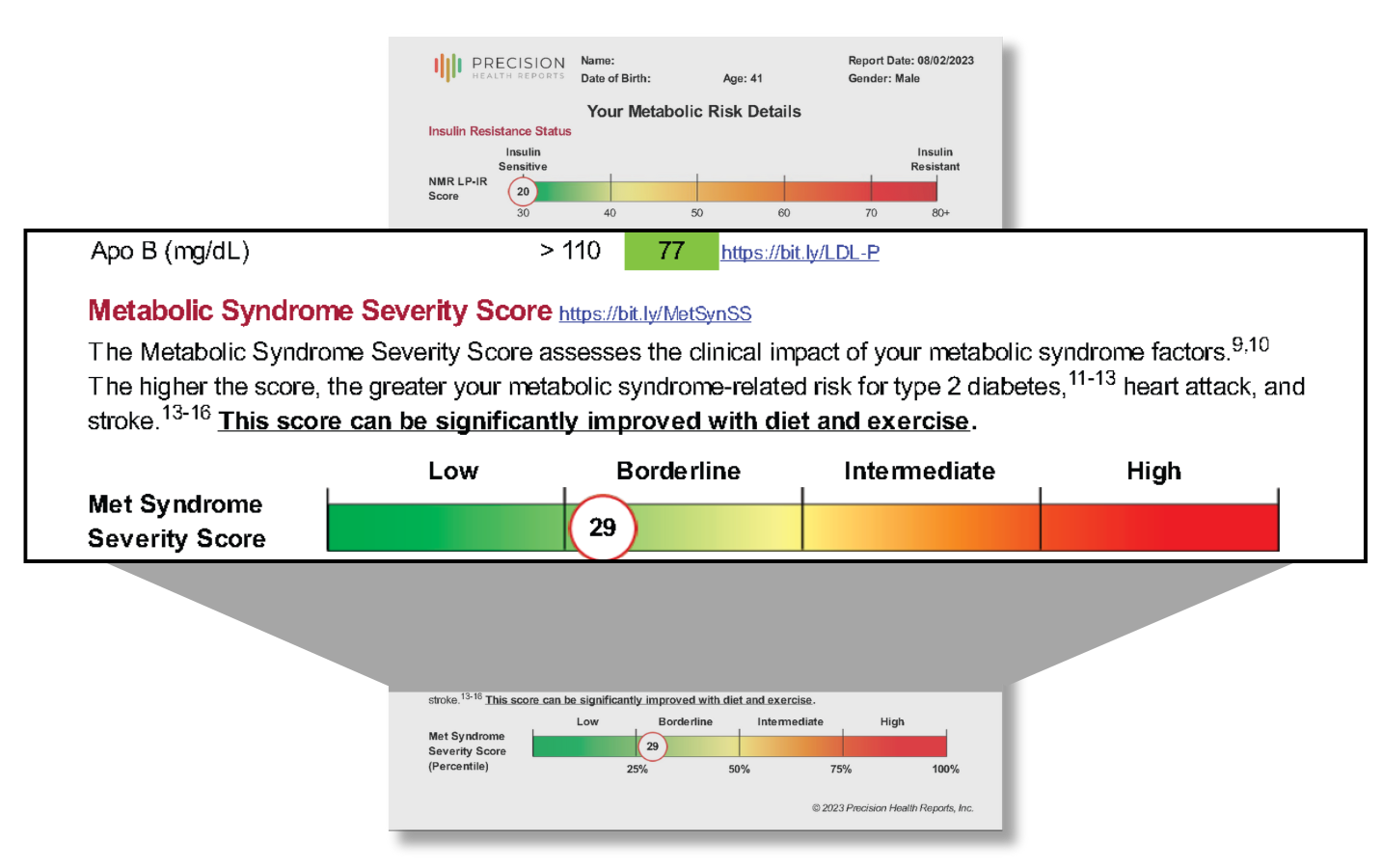
At Precision Health Reports, we integrate both the traditional diagnostic criteria and the MSSS into our Cardiometabolic Risk Assessment, alongside advanced biomarkers such as ApoB, LP-IR, GlycA, and Lp(a). This approach allows us to deliver individualized, guideline-based prevention plans that go far beyond routine lab testing. Here is what you see in a Cardiometabolic Risk Assessment or an Advanced Metabolic Health Assessment report:
How Is Metabolic Syndrome Diagnosed (Traditionally)?
Metabolic syndrome traditionally gets diagnosed by a cluster of five cardiometabolic risk factors. According to the ATP III and AHA/NHLBI definitions, metabolic syndrome is diagnosed when a person has three or more of the following:
Abdominal obesity: waist circumference >40 inches (men) or >35 inches (women)
Elevated triglycerides: ≥150 mg/dL
Low HDL cholesterol: <40 mg/dL (men) or <50 mg/dL (women)
Elevated blood pressure: ≥130/85 mmHg or on antihypertensives
Elevated fasting glucose: ≥100 mg/dL or on glucose-lowering medication
This “checklist” is practical, but overly simplistic. It provides a yes/no diagnosis without acknowledging that metabolic syndrome exists on a spectrum of severity. Someone can have elevated or high risk for being metabolically unhealthy but still have less than 3 features of metabolic syndrome meeting the general criteria. This is a problem.
Why Metabolic Syndrome Matters—A Lot!
Increased Risk for ASCVD
Metabolic syndrome nearly doubles the risk of heart disease. The combination of dyslipidemia (high triglycerides, low HDL), hypertension, and insulin resistance accelerates the development of atherosclerosis.
Strong Predictor of Type 2 Diabetes
People with metabolic syndrome are five times more likely to develop type 2 diabetes compared to those without it.
Connection to Systemic Inflammation & Insulin Resistance
Metabolic syndrome reflects a deeper underlying biology: insulin resistance, systemic inflammation, and adipose dysfunction. These processes fuel not only diabetes and ASCVD, but also fatty liver disease and other metabolic complications.
👉 For more information about insulin resistance measurement, see our guide on Why Use LP-IR vs. Fasting Insulin?.
Limitations of the “5 Features of Metabolic Syndrome” Checklist Approach
While widely used, the checklist diagnosis of metabolic syndrome has two key limitations:
Binary classification: Patients either “have it” or “don’t,” with no gradient of severity.
Poor predictive resolution: Two people can both meet criteria but have very different risks.
This oversimplification can cause clinicians to miss high-risk individuals who fall just short of the cutoff, and it cannot measure whether someone’s risk is getting better or worse over time.
The Metabolic Syndrome Severity Score (MSSS)
What Is MSSS?
The Metabolic Syndrome Severity Score is a continuous variable score from 1-100 that quantifies the severity of metabolic syndrome. It incorporates the same five core variables (waist circumference, triglycerides, HDL-C, blood pressure, fasting glucose), but weights them differently based on:
Sex (male/female differences)
Race/ethnicity (Black, White, Hispanic-specific weighting)
This approach was developed using NHANES population data and validated in multiple cohorts.
Why MSSS Is More Powerful
Continuous measure: MSSS ranges across a spectrum, avoiding the limitations of “yes/no” diagnosis.
Predictive accuracy: Higher MSSS values are strongly associated with future type 2 diabetes and ASCVD events.
Trackable: MSSS can be used to monitor whether a patient’s risk improves with lifestyle changes or treatment.
Tailored to individuals: Sex- and ethnicity-specific scoring improves accuracy and clinical relevance.
Curious where you stand? Use our Metabolic Syndrome Severity Score Calculator.
👉 For more information about advanced cholesterol testing, see our article on Understanding the NMR LipoProfile.
Clinical Evidence Supporting MSSS
Diabetes risk prediction: Gurka et al. (2016) showed that MSSS strongly predicts incident type 2 diabetes, outperforming binary diagnosis.
CVD outcomes: DeBoer et al. (2017) found that higher MSSS correlates with increased risk of ASCVD events.
Broader cardiometabolic outcomes: MSSS has also been linked to chronic kidney disease, fatty liver disease, and systemic inflammation.
In short, MSSS provides a quantitative, evidence-based way to predict outcomes and personalize care.
How Precision Health Reports Uses MSSS
At Precision Health Reports, we believe patients deserve both clarity and precision. That’s why our Cardiometabolic Risk Assessment integrates:
Traditional checklist criteria for clear diagnosis and commonality to standard practice.
MSSS for continuous, individualized severity measurement and to build clinical awareness of this more advanced method.
Advanced biomarkers:
ApoB → reflects atherogenic particle burden which confounds with metabolic syndrome to increase risk for diabetes and ASCVD events.
LP-IR Score → advanced measure of insulin resistance.
GlycA → markers of systemic inflammation.
This combination allows us to:
Identify patients who might otherwise be missed.
Provide personalized thresholds and treatment targets based on guidelines from the ACC, AHA, ESC, and NLA.
Track individual progress over time, not just “yes/no” diagnosis.
👉 For more information about ApoB and Lp(a), see our article on ApoB and Lp(a) Testing.
Why Metabolic Syndrome Severity Score Integration Matters for Patients and Clinicians
The integration of MSSS into risk assessment has three major benefits:
Better risk detection: Identifies high-risk patients earlier.
More precise management: Guides LDL-C, ApoB, and glucose targets based on severity.
Motivational tracking: Patients can see their MSSS improve as lifestyle or therapies take effect. Progress is motivating!
Curious where you stand with regard to your own Metabolic Syndrome Severity Score? Use our Metabolic Syndrome Severity Score Calculator.
👉 For more information about setting personalized lipid targets, see our article on LDL-P and Cardiovascular Risk.
Prevention and Management Strategies
Whether diagnosed by the checklist or quantified by MSSS, management of metabolic syndrome involves:
Lifestyle optimization: weight loss, nutrition, physical activity, stress management.
Pharmacotherapy when needed: statins, antihypertensives, glucose-lowering therapies.
Ongoing monitoring: repeat MSSS + biomarkers to track whether interventions are lowering risk.
At Precision Health Reports, we deliver a personalized report to develop an action plan for each patient, aligning with clinical guidelines but tailored to their unique profile.
👉 For more information about improving overall risk prediction, learn Why Measuring Cardiometabolic Risk is Important.
Key Takeaways
Metabolic syndrome is a powerful risk identifier, but the traditional checklist oversimplifies risk.
The Metabolic Syndrome Severity Score (MSSS) offers a continuous, validated, and trackable measure of severity.
Precision Health Reports integrates MSSS, traditional criteria, and advanced biomarkers to deliver personalized, guideline-based prevention strategies.
👉 Ready to see your personalized risk? Learn more about our Cardiometabolic Risk Assessment.
FAQs
Q1: What is the Metabolic Syndrome Severity Score (MSSS)?
The MSSS is a validated, continuous score that quantifies the severity of metabolic syndrome based on waist circumference, triglycerides, HDL-C, blood pressure, and fasting glucose, adjusted for sex and race/ethnicity.
Q2: How does the MSSS improve on the traditional diagnosis?
Unlike the binary checklist (yes/no), MSSS provides a continuous measure, tracks changes over time, and better predicts future diabetes and cardiovascular events.
Q3: Is MSSS used in clinical practice?
Yes. Multiple studies published in J Clin Endocrinol Metab, Circulation, and J Am Heart Assoc demonstrate MSSS as a strong predictor of cardiometabolic outcomes. PHR incorporates it directly.
Q4: Can MSSS help track improvement?
Yes. Because it’s a continuous score, it shows whether lifestyle changes or treatments are lowering risk over time.
Q5: How does Precision Health Reports use MSSS?
PHR combines MSSS with traditional diagnostic criteria and advanced biomarkers (ApoB, LP-IR, GlycA, Lp(a)) to provide a comprehensive, personalized risk assessment and management plan.